In December of 2020, as a deadly Pandemic swept across the country, a pandemic the likes of which has not been seen since the Spanish Flu one hundred years past, I went to a substance-abuse and addiction treatment center in central Florida for five weeks. Here’s what I packed for my time there:
A few lightweight blouses. Not enough winter clothes. A lifetime of cumulative guilt, anxiety and depression. A history of psychiatrists, psychologists, therapists, and counselors. A growing abuse of alcohol and prescription drugs. A paperback novel by Alice Hoffman, in case I learned to read with focus again. A little makeup. My new iPhone 11. A worn out pair of running shoes. A history of literal and figurative running along paths leading nowhere and everywhere. Flip flops. Sweat pants and blue jeans. And a belt, which I needed because I’d lost 30 pounds in about 3 months, and my jeans would fall to my knees without it. A sketchbook, a couple of brushes, three tubes of watercolor paint, and a bag of colored markers. Suicidal ideation. Socks and underwear. Fear. Despair.
I have struggled with mental illness and depression for most of my life. At 19 or 20, I saw a psychiatrist and was was diagnosed with Obsessive-Compulsive Disorder, not to be confused with the “OCD” that some folks claim with an eye-roll and a chuckle because they wipe down their counter tops twice. This disease took over my life, although it would go into remission at times and allow me to live my life “normally.” The Irrational fears and compulsions that took over at times were debilitating, but usually I pushed through the days, going to college classes, getting a degree, getting married, finding a job, working as a server, then a teacher, maintaining as much normalcy through it all as possible.
But at times the depression and fear that accompanied my OCD would make me realize it might have been active for two years or longer, and I’d feel trapped by it, hopelessly wondering if things would ever improve. I was in and out of therapy most of my life. Sometimes it helped, but never enough.
When antidepressants came along the trail of science, I tried many, but could never get past the initial side effects. Then finally, when told to try a new one specifically tailored to help with intrusive thoughts, I stuck through the worst of those effects with a drug called Luvox. My new psychiatrist had come through for me, and I had some measurable relief for about 10 years. I was grateful that it came during the period of my mother’s decline into dementia, and her subsequent five-year tenure in an Alzheimer’s care unit. The relatively small amount of Xanax that was this doctor’s other “gift” to me seemed to help too. I started taking a little to help get me back to sleep at night. When I’d begin to worry about the amount I was taking, both my doctor and the pharmacist assured me it was safe and manageable.
Then, about four or five years after Mom’s death, the Luvox stopped working. That drug and prescription Xanax had gotten me through the worst of my mother’s illness and death. After that, when the Luvox wore off, I leaned more and more heavily on Xanax, a substance in a class of drugs known as benzodiazepines, which also includes Valium and Ativan.
Around 2018, I spiraled deeper and deeper into depression. Yet another psychiatrist (the old one had segued into administration, and the one replacing him, a woman I liked, moved on as well) prescribed more antidepressants; they did nothing.
By then I’d been diagnosed with “Serious Depression Disorder.” My doctor suggested ECT treatments: Electro-Convulsive shock Therapy, which he would administer there in his office. They leave the word “shock” out of the acronym, perhaps to cushion the blow of hearing such a suggestion.
I had seventeen of those treatments. We’d go about every week. My husband drove me to all of my appointments ninety minutes away in Birmingham for two reasons: I was no longer able to function well enough to drive my car, and I was completely out of it afterwards.
Finally, my husband Stephen, who’d researched ECT treatments and found that fourteen was actually the recommended cut-off number, confronted my doctor with the fact that I’d had one or two over that boundary. However, Dr Farley (not his real name) said we should “continue them until they work.”
Soon after that, my husband sat next to a gentleman in the psychiatrist’s waiting room, who told him, “You know, I’ve been bringing my wife here for 2 years for these treatments. And I don’t think they’re helping her.” Stephen ran this by me, and I decided I’d had enough.
“I think they made you worse,” Stephen said later. He also told me how devastating it had been to watch me emerge from each ECT treatment, my cognition impaired enough to make me stagger toward him, asking questions he’d answered just a few minutes before I’d ask the same one over again. Once it was, “When am I supposed to get my treatment?”—right after we got in the car to go back home from a treatment.
I believe now, fervently and with conviction, that this doctor was a total quack, in it for whatever money he could make. And I was collateral damage along with that other poor guy’s wife.
We decided to stop going for those treatments, but I continued to see Dr. Farley, I suppose out of desperation, and certainly a need to continue my Xanax prescription. I also began to drink more and more at night, and then during the day. I started falling from the combination of alcohol, Xanax, and other drugs. I went to a new therapist who told me I needed to go to a substance-abuse treatment center. I chose to ignore her and refused to go back.
I passed out and fell on my face one night in my kitchen, bursting an artery in my nose and biting through my upper lip, shredding it “like hamburger,” according to the plastic surgeon who had to stitch it together. My husband, who was told later that had he waited for an ambulance I might well have bled to death, literally saved my life that night, rushing me to the hospital where I spent 4 days and had plastic surgery on my nose as well as my lip. Xanax and the alcohol I’d been using along with it were found in my blood; this went on record at the hospital, a record which eventually ended up on Dr. Farley’s desk as a “heads-up” about this particular patient: me.
I got out of the hospital, but then I went home and took my Xanax, washed it down with wine, and fell again not long afterward. My husband had had to call the paramedics more than twice in the recent past, once because I’d finished off a fifth of liquor and was losing consciousness, dangerously close to alcohol toxicity, but when I’d get out of psychiatric lock-up or the hospital, I’d begin the cycle again. One night (among many) when I became frightened of the urge to kill myself, Stephen called a friend in the mental health field who suggested I go to a Birmingham hospital and check into a room for focused treatment. But when we got there, there were no rooms. There was Covid blooming like a poisonous rose garden all over the state. We waited for hours. And hours.
Finally I couldn’t take it any more, the endless waiting, the sterile room filled with hurt people, many needing rooms that were not there.
“I have to get out of here,” I told my husband. We got up to go and headed out the door. Two security cops suddenly blocked our way.
“She’ll leave when we say she can leave,” one of them said. He knew I was a suicide threat: I’d put that on the form. I froze, a deer caught in headlights, and looked at Stephen, this man I’d put through so much. He met the cop’s gaze evenly and shot back, “We’re leaving. You’ll have to come through me to get to her.” He’s 6’4, weighs 235 and is fiercely protective of his family. They let us pass, but one of them followed us out to the parking deck. “You should think of her well-being,” he said. If he only knew.
My next appointment with Dr Farley involved his informing me that he’d have to limit my Xanax (“There was a fall? Is that right?”—as he glanced at a piece of paper on his desk). I’d been caught out. That was the day I learned exactly how Heath Ledger had died, as Farley blasély informed me that mixing alcohol and Xanax was what had killed the actor. But as I’d pushed so many other blatant warning signs away, I shoved this one from me as well. I know now that I wanted to die, and that I was working subconsciously or consciously on making that happen.
In fact, eventually, I had a Plan. It was a very detailed plan, and I also had a back-up plan. And my poor husband and other family members knew I was considering suicide. They loved me, but several told my husband to leave me for his own well-being. I don’t blame them. I wanted him free of me. I wanted
ME free of me.
But he stuck it out, and continued the research into my condition and possible treatments; he took me to Dr. Farley until we both realized the fruitlessness of that travesty.
And then, one day in October or November of 2020, I told my husband I couldn’t take it any more. I’d been sinking steadily toward dying of drug and alcohol addiction for well over two years, and I was only getting worse. He asked me if I was ready to do something about it, and desperate, curled into a fetal position, weeping, I agreed to go into detox. Stephen found a place and made me an appointment for about a week later.
I spent the next days wondering what was going to happen to me. And so I began drinking as soon as I woke up in the morning at that point, right up until I went to Detox at a medical center in Jackson, Alabama, where they gave me other drugs to help me off of the problematic ones. I felt numb the entire time, cushioned in the white terrycloth robe I’d packed, sort of swaddled in heavy cotton and drugs.
The week after I got out of the hospital in Jackson was the most horrific week of my life. I’d begun to wake in the middle of the night, terrified of something I couldn’t define. I’d go into the bathroom, raise the window, let in the icy air, and smoke cigarettes, deeply inhaling smoke, terrified I might put my now-defined Plan in action. I stared at some sharp nail scissors on the counter, but I had a recurring image of myself driving my car less than half a mile away, out into the woods that surround our very rural house, packing a bottle of Vodka, as many pills as I could find, and something very sharp. Then I’d go to work, veiled by a dark forest, sheltered by pine trees alongside an overgrown path tapering off as it led into darkness. I’ve never had a more terrifying experience than those nights during the week between Detox and Rehab.
So that, and feeling like I owed another effort to my husband, led me to an addiction and treatment center he found on line, in central Florida. I went there for 5 weeks.
And there, although I technically do not believe in miracles, I feel they worked one on me. There I learned first that I had to get help not for my husband, not for my elderly father, my brother, not for my friends. I had to get help for me. Because I mattered. I was worth saving. Another gift they gave me was the desire to help others who’d lived through similar struggles and fears.
At this Treatment Center, Laketree Oaks (not its real name) I learned valuable tools and principles of healing and recovery. I learned these not only from the staff, most of whom were recovering addicts themselves, these psychiatrists and doctors and therapists; I also gained insight and support from the other clients. They were mostly younger than I, kids really, or so I labeled some of them who were of course really young adults struggling to survive.
My roommate Melody (not her real name) was someone I connected with instantly and who was always there, awake in the middle of the night, always willing to talk and listen through my night fears, which hadn’t gone away. I guess there were four or five nights that I’d come awake with a jerk, like I had the week before leaving, clawing at a name for the terror consuming me. At first, in trying to define my worst fear for my therapist there, who asked me that specific question at one of our first sessions, I thought it was fear of dying, the fear that I would end my life somehow, maybe even while I was at the center. Then I thought it was a terror of not being in my right mind, like what had happened to my mother before she died. Then it was an un-named potential buried deep in my brain, the Fear of Fear itself, I suppose.
I’d begun to awaken between 2:00 a.m. and 5:00 a.m when I was tapering off some of the stronger drugs they’d given me to help with withdrawal. And there was Melody in the bed by the window, a dark shape under a blanket. I’d softly ask her, “Melody…are you awake?”
She was. She was always awake or came awake fluidly in the instant, magically it seemed, alert and ready to listen, and then her soothing voice would speak exactly the right words, words I hadn’t even known I needed until she spoke them. I believe she was as valuable in those moments and beyond them as my therapist there was to me, and that particular woman was also excellent at what she did. Melody would respond in an instinct-driven fashion to my exhausted expressions of fear. These were often connected to the obsessive guilt-ridden intrusive thoughts that were hallmarks of my particular brand of OCD. I’d hold my breath at times, worried sick as I had in the past that I’d risked some sort of judgment from the listener, something that would only increase the guilt. I’d once told a therapist something extremely difficult for me to admit, and he’d laughed.
But Melody never blinked. She just spoke in her quiet lovely voice to me as she gently, firmly, soothingly, said exactly the right things. They were simple observations, but they felt like magic words to me at the time. In fact, I believe with all my heart now that there was something like magic involved with the fact that we became roommates while we were there. I am twenty-five years older than she, but there was and still is no age difference between us at all. The most powerful magic, though, came one night in the form of a dialogue unlike any I’ve ever had with anyone, when in response to my awakening yet again, filled with that sharp yet murky unidentifiable fear of myself, she shared this story:
One night, many years ago, she’d been with others at a meeting that focused on principles of Dharma and meditation for solace, and during a break, had spoken with an old man she’d met there about her own fears and self-doubts. He was a practicing Buddhist, and he’d given her this adage in response: “I am not my mind. I am not my body.” She’d found great power and solace in those words, so much so that she’d had them tattooed on her forearm.
I repeated the words she’d just gifted me: “I am not my mind. I am not my body.” I knew something about Buddhist philosophy at this point, as I’d been joining the Dharma/Meditation group there at the Center on a nightly basis since I’d learned of its being an option to the AA meetings. I’d been to one of those, and had found it a strangely unsatisfying experience. So I went to learn how to meditate instead, which turned out to be as strangely satisfying, and rather powerful. So I knew, suddenly, where this adage might take me. I knew that if I wasn’t my mind, if I wasn’t my body..
“So…I am my soul?”
“Yes,” Melody replied.
“And my soul.. is Love.” I concluded. So simple. Yet infinitely complex. Suddenly, though, it made sense. In daily instructive group sessions, we’d learned so much of the importance of Community. Of the importance of helping others, of channeling an unchanneled potential for love into definable, tangible places: we’d relearned and reemphasized the importance of connecting with others, with the Human Family, and giving the gift of ourselves. I’d already realized the impact and value of giving through teaching. That the rewards really so often do outweigh the stresses and strains of the giving process. That caring for others is perhaps as important as caring for the self, perhaps central to caring for the self.
And so, it all suddenly came to a head as it came into MY head. I simply HAD to refocus. I was NOT my mind, turbulent and in turmoil from fear of my Self. I was NOT my body, threatened by my mind with its permanent cessation by suicide. I was my Soul. And I knew how to Love. In that way, I could set my Self free. After that night, I never woke in fear again.
Melody had told me something that was to become woven into another story I’d retell later, my last night at the Center, a story I’d put to music. I was to use this story in what was an apparently powerful form of meditation shared to help my friends there, friends who had become my family, to heal themselves in a way similar to the way Melody had helped me to heal.
About the same time, I was to learn from my therapist there that the night fears were actually PTSD stemming from Xanax withdrawal, and might continue for 2 more years (they didn’t, thank all the powers of the Universe). It was a relief to know this, like naming the Devil.
My therapist, Jane (not her name) along with Melody, helped me understand myself in bursts of enlightenment that no one else has ever come close to producing before. With all of the hours and hours of therapy that contribute to the comprising of my life experiences, the talent this young woman honed into the success story that is my story is unprecedented and unparalleled.
Jane made every minute of our hour-long weekly sessions count, and then she gave me homework. She re-awakened the joys of research I’d discovered in grad school as I wrote term papers on Hemingway and Styron. Now I was researching the philosopher Carl Jung and writing imagined dialogues between my mother and me, conversations we’d never had that I longed for and used as a powerful tool for self-discovery. Jane helped me realize what I’d always suspected: the past WAS important; the present WASN’T all that mattered, the reverse being an aspect of contemporary thinking that I believe many modern therapists hold dear. And she helped me assuage the terrible irrational guilt that had plagued me off and on all my life. She helped me lay it to rest, and keep it at bay, maybe forever.
I will tell you with honestly that this therapy was almost like great sex, where one says, “Wow. I didn’t know it could be like that.” This is what a good therapist can do for someone. For someone like me, who’d decided jadedly some time ago that therapy was truly overrated and definitely overpriced, it was a true epiphany.
Another perk of the program was the busy schedule beginning early in the morning, consisting of five or six classes spread throughout the day. Many of the teachers were recovering addicts themselves, determined to help with the healing of others as a part of their own ongoing recovery. I learned about Cognitive Behavioral Techniques, involving re-conditioning one’s self to think differently, to break out of harmful approaches to thinking about situations and one’s response to them.
I also attended health classes daily, and in several of these I learned things I wish I’d known decades earlier, things I had not associated with learning in a “health class.” But health relates to the mind as well as the body. And one day in particular I learned that the type of OCD I had could involve having a very obsessive kind of intrusive thinking that had been so difficult for me to confront—so devastating and demoralizing to even acknowledge to anyone—that I began to fear it might not actually be a part of the illness.
I was terrified that it might actually be a part of me. I learned that day that it was NOT unique to me. And the relief I felt almost brought me to my knees. What there is out there to learn about one’s self is enormous, and can help to put you on the road to healing, to redemption, back to peace, back to the ability to love others, and to be loved for who you really are again.
Eventually, although I was scheduled to leave at the end of a month’s time, I decided I needed another week at the Center to tie up some loose ends. Melody had gone. We’d arrived within a day of each other, and both of us had contracted to stay thirty days, so her month was up. I wasn’t sure I’d be okay without her, but as it turned out, I was.
My meditation/Dharma group had been a central part of healing for me. The breathing exercises, the other relaxation tools, the recordings of narrator-led journeys to places enhanced by our imaginations, the beautiful traditional meditative music played to help relax us; all of these elements came together to take me outside of my exhausted mind and help me find solace and a measure of peace.
When the other 10-20 meditation-group members found out when I was scheduled to go home, one of the leaders suggested that I might like to lead the group in meditation the night before I left. I was honored. He said he’d help, and other friends, among them Eva, a beautiful young transgender woman who’d become a dear friend, offered to help as well. I went back to the room and began to write. I decided to tell Melody’s story and what that story had done for me, and the story flowed from me like liquid gold.
That night, when I finished sharing my story and Melody’s, Eva brought the group back to themselves with more “awakening”
techniques. It was dark in the room. I could hear a few people crying softly. And there was a good bit of hugging that followed, and some requests for the story and music to be sent to people’s phones. I was gratified at the reception. I couldn’t wait to tell Melody how her story had become mine.
Melody and I are still in close contact almost 2 1/2 years later. She does her own thing to try and work the program where we met: she’s involved in non-profit groups that extend to situations often involving the Criminal Justice system and how it can be for those addicts who’ve found their way inside that system.
She’s every bit the sharply intuitive and loving person she was for me in my time of need, and she is more, thanks to LakeOaks. The world is lucky to have the Melodys within its communities, caring enough to give time and self to helping others.
Why am I telling you this? All of this deeply personal stuff that observers and onlookers often find shameful? I am a recovering addict. I know I’m taking a risk in sharing so openly. There is a stigma that comes with being mentally ill, and certainly with being an addict, even in recovery. Often, there is judgment. Sometimes, people laugh at you when they don’t know any other way to react. I am ready for all of it. And often, there is shame.
But I am no longer ashamed. I hope with all my heart that there are readers out there who will find some hope in something I’ve shared here. Who will understand that there may be help out there that actually works, that a complex combination of elements worked to help me with my set of complex combined problems.
And yes, it did cost money. It was my Privilege that enabled me to go to this treatment center. Many people suffering from mental illness and the self-medication and addiction that so often accompanies it either keep doing what works to help them get some relief, or they descend into the kind of isolation and despair that I experienced, or both. And often, there don’t seem to be viable answers. Some meet with a terrible fate that most of us cannot even imagine.
The recent death of a mentally ill incarcerated man in Jasper has been the focus of family and other residents since his terrible demise. I know that this man’s family is suffering terribly as a result, and my heart goes out to them. That family’s efforts to help this young man spiraled into a nightmare that they could not have possibly predicted. It is my fervent hope and prayer that ongoing investigations into Tony Mitchell’s final days produce some sort of eventual closure to questions that have arisen as to the exact nature of this man’s death. This is an event that has come together with other motivations inspiring me to share my own experiences with mental illness and addiction.
There are solutions. However, they can be very difficult to find. There are good therapists out there. And there are bad ones, too, unfortunately. Vetting a therapist can be a challenge, but if you’re looking for a good one, it pays to read reviews. And of course, talk therapy, like physical therapy prescribed for some health conditions, is often expensive and is often not covered adequately by health insurance.
And often, the kind of treatment center that I went to for five weeks is not an affordable option. However, as a retired public-school teacher who was never really into teaching “for the money,” I can tell you this: these places often reduce their rates in certain cases; in my case, in December of 2020 through January of 2022, the center was running a “Covid Special” that I took advantage of. I had some savings, and even at the special rate my stay depleted a good chunk of them. It goes without saying that it was well worth the money for me. And insurance certainly can help; many of the clients there were covered to some extent by their insurance plans. It all depends on type of insurance and what’s accepted at individual centers.
And there are smaller, much less expensive local treatment centers available to those in need. It is the focused attention at all of these centers, large and small that is so powerful. It’s the staff, the types of therapy, the activities and programs offered within each; the educational resources, and the other clients as well that can combine to create an atmosphere that can be conducive to healing and recovery.
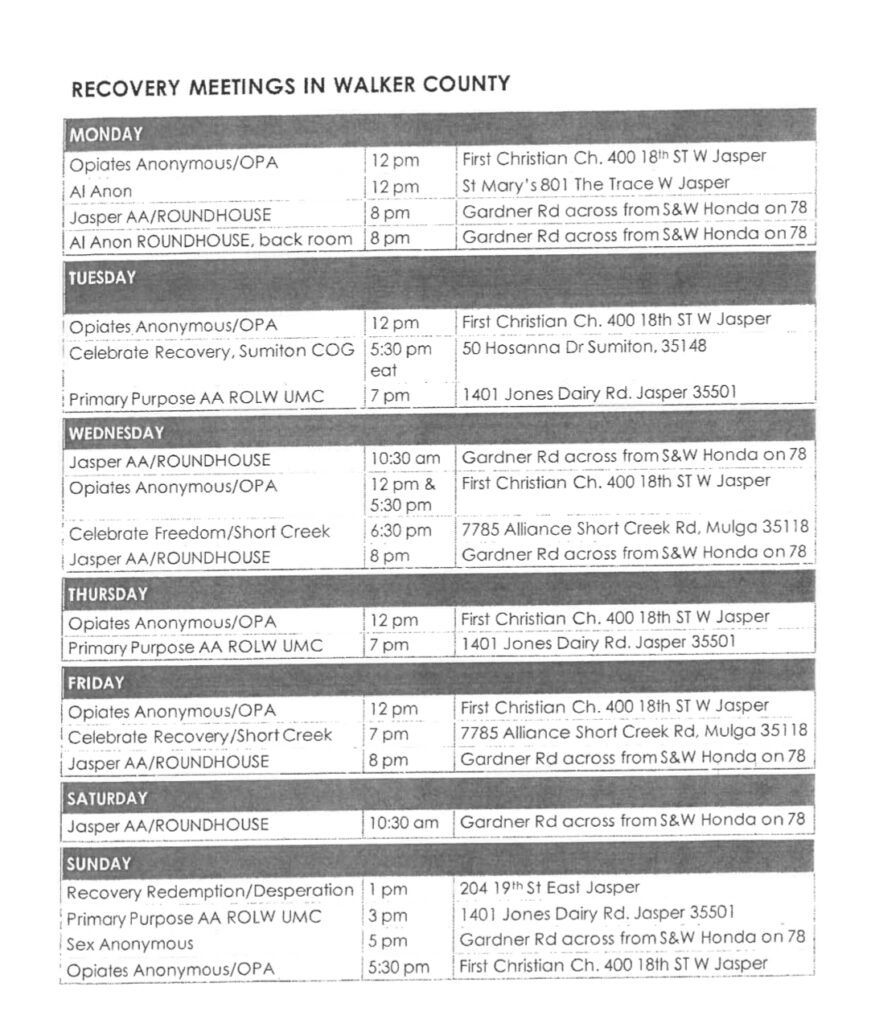
This article concludes with a list of local active centers in Walker County and in surrounding areas. If only one person decides to explore the options for a family member, for a friend, or for one’s self, the effort invested in writing and publishing this article will have been well worth the effort.
The effort of writing this out alone has been a huge part of my own ongoing therapy. Other efforts involving community outreach have also helped since I left my Treatment Center in Florida. I am still a part-time teacher: I work at my local arts center with children and adults who want to learn how to draw and paint. And that is something I enjoy a great deal.
I am also an artist and a writer. Since the Pandemic and my concomitant descent into my own version of Despair, my focus, however, has gone from a desire to market my work for profit to what I consider a greater calling: The hope of helping my community. The hope that reaching out to others in some small way, like writing this article, might have life-changing results.
Because I DO believe that I am not my mind, that I am not my body, that mind and body are small parts of a much greater and holistic Whole. I believe that each of us has a Soul, and that no matter what belief system you embrace, they all have this in common: The Soul is Love.
Janet Mego is a retired Walker-county public-school English teacher, currently filling her time as a writer, artist and part-time art instructor. You may reach her at janetmego@gmail.com.
List of Resources:
Local Recovery Meetings:
General Resources:
1) Addiction Center Services:
844-548-1118
2) Awakening Recovery
205-295-2336
3) Hope for Women
https://www.hopeforwomenllc.org
205-265-2799
4) Kolbe Clinic
888-310-9011
5) Walker Recovery Center
205-221-1799
6) Paces For Parents
https://www.stepsproactiveparenting.com/WalkerCoPACES
7) Serenity Lodge Detox/Admissions Hotline
8) For further information on Drug Rehab Centers in Walker County, AL:
https://www.addicted.org/walker-county.html
This link led the author to her Treatment Center:
https://americanaddictioncenters.org/addresses
1-800-662-4357 SAMHSA HELPLINE